Healthcare Claims Management Services
At our healthcare claims management services, we specialize in optimizing your revenue flow through accurate claim processing, proactive follow-up, and compliance assurance.
- Optimized Claims
- Efficient Processing
- Claim Accuracy
- Home
- Revenue Cycle
- Revenue Cycle Operations
- Claim Submission
Why Outsource Healthcare Claims Management
Outsourcing healthcare claims management is a smart choice that can greatly benefit healthcare providers. It enables providers to prioritize patient care activities while ensuring a smooth revenue cycle management process. By relying on experienced professionals in claims processing, providers can optimize operations, minimize administrative burdens, and enhance overall financial performance.
Outsourcing healthcare claims management also brings a high level of proficiency and deep understanding of the industry, guaranteeing accurate and timely processing of claims while adhering to constantly evolving healthcare regulations. This external support not only improves operational efficiency, but also helps to minimize errors, reduce claim denials, and ultimately maximize revenue for healthcare practices.
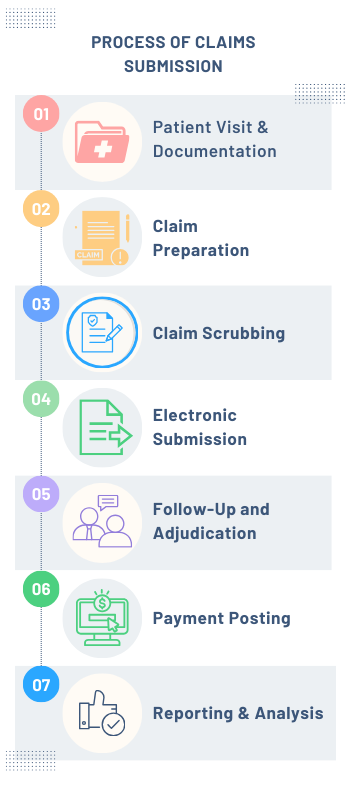
Our Proactive Approach towards Claims Submission Process
Step 1. Patient Visit and Documentation
Our team is highly skilled in accurately documenting medical services provided during patient visits. This includes precision capturing of patient details, diagnosis, and procedure codes.
Step 2. Claim Preparation
Our team of highly skilled professionals carefully prepares the claim, paying close attention to precise coding, meticulous formatting, and strict adherence to payer guidelines to ensure optimal reimbursement.
Step 3. Claim Scrubbing
Our thorough scrubbing process ensures that every claim is carefully reviewed and corrected for errors or discrepancies, guaranteeing a smooth and efficient submission process with minimal risk of denials or delays.
Step 4. Electronic Submission
Our team utilizes advanced technology to submit claims electronically to insurance payers. This ensures a streamlined process and reduces the chances of errors, leading to efficient processing.
Step 5. Follow-Up and Adjudication
Our team is highly skilled in handling claims and promptly addressing denials or delays. We are committed to promptly resolving issues with payers.
Step 6. Payment Posting and Reconciliation
Our expertise in claim submission ensures that payments are accurately posted and reconciled with your records. Any discrepancies that may arise are promptly addressed to maintain financial accuracy.
Step 7. Reporting and Analysis
Our comprehensive reports offer valuable insights into claim status, reimbursement rates, denials, and other important metrics. With this information, you can effectively monitor performance, identify changes, and make well-informed choices that improve the efficiency of your revenue cycle management.
Say no more to endless paperwork and delays – our automated claims management system streamlines the entire process. Get in touch to get more info [+1 (978)-709 1991].
Key Features of Our Healthcare Claims Management
Our dedicated team prioritizes accurate coding, meticulous documentation, and adherence to payer guidelines to optimize reimbursement.
Our expertise lies in electronic claim submission, where we utilize modern technology to accelerate the method of submission, minimize errors, and enhance efficiency in processing.
Our services prioritize strict adherence to healthcare regulations and payer guidelines, guaranteeing full compliance in all claims management aspects to minimize potential risks.
We carefully review each claim to identify and correct errors, guaranteeing accurate claim submission and minimizing denials.
We take the initiative to promptly address any claim denials or delays, ensuring that payers quickly resolve them for optimized revenue flow.
Our team of dedicated professionals is here to provide you with personalized assistance, industry knowledge, and a strong commitment to delivering top-notch healthcare claims management specifically tailored to meet the unique needs of your practice.
Testimonial
Dr. Cameron Everly, Medical Director
Want to ensure accurate claims processing every time? Put our experienced team of specialists to work for you. Call us at +1 (978)-709 1991 to get started!
Benefits of Our Healthcare Claims Management Services
Our services ensure accurate claim preparation and submission, leading to improved reimbursement rates and increased revenue capture for your practice.
By leveraging our expertise in claim scrubbing and validation, we minimize errors and discrepancies, resulting in fewer claim denials and faster payment processing.
Experience streamlined operations with our efficient claim submission process, allowing your staff to focus on patient care while we handle the complexities of revenue cycle management.
Timely follow-up on claims, prompt resolution of issues, and optimized reimbursement processes contribute to improved cash flow and financial stability for your practice.
Our services prioritize adherence to healthcare regulations and payer guidelines, ensuring compliance in all aspects of claims management and reducing the risk of penalties.
Benefit from customized reporting and analytics that provide valuable insights into claim status, reimbursement trends, and performance metrics, empowering data-driven decision-making for your practice.
With our dedicated team of professionals, you receive personalized support, industry expertise, and a commitment to excellence in healthcare claims management, tailored to meet the unique needs of your practice.

Frequently Asked Questions
Claims management in healthcare involves the process of submitting, processing, and managing medical claims for reimbursement from insurance payers. It includes tasks such as claim preparation, submission, follow-up, and resolution of denials.
Claim processing in healthcare refers to the systematic handling of medical claims from submission to payment. It involves verifying patient information, coding services, submitting claims to payers, and reconciling payments.
The types of claim submission in medical billing include paper claims, electronic claims (EDI), and web-based claims submission. Electronic submission is the most efficient and widely used method in modern healthcare billing.
The first step in processing a claim is accurate documentation of the medical services provided during the patient visit. This includes capturing patient details, diagnosis codes, procedure codes, and any other relevant information for claim submission.
Outsourcing claims management can benefit your practice by improving revenue capture, reducing claim denials, streamlining operations, ensuring compliance, and providing access to specialized expertise for efficient revenue cycle management.
Technology plays a crucial role in healthcare claims management by enabling electronic claim submission, automated processing, real-time tracking, data analytics for performance insights, and ensuring secure and efficient communication with payers.
We ensure compliance with healthcare regulations by staying updated on industry standards, adhering to payer guidelines, conducting regular audits, maintaining accurate documentation, and implementing robust processes to mitigate compliance risks in claims management.
Let’s start a
conversation
We’re here to help you find out how Healthcare Claims Management Services could benefit your practice. Complete the quick form to the right, and someone will reach out to you soon.
Our Experts will:
- Discuss your individual use case and business needs
- Explain our features, benefits, and services
- Show how this solution can help achieve your goals